Seoul National University Hospital Demonstrates Potential of AI to Predict Antiepileptic Drug Response
- Input
- 2026-01-09 09:26:26
- Updated
- 2026-01-09 09:26:26
[Financial News] A Korean research team has presented an artificial intelligence (AI)-based analytical model that can predict, early in treatment, which antiepileptic drug will be most effective for a patient with epilepsy. The model is drawing attention for its potential to overcome a key limitation of current practice, in which drug response can only be confirmed after the medication has actually been administered. The research team led by PARK Kyung-Il and Professor Sang Kun Lee of the Department of Neurology at Seoul National University Hospital, together with Prof. Young-Gon Kim of the Department of Convergence Medicine, announced on the 9th that they had used a machine-learning model trained on 84 clinical variables to predict treatment response to individual antiepileptic drugs.
The study is particularly significant in that it utilized the largest single-center epilepsy cohort database in Asia.
Epilepsy is a disorder characterized by recurrent seizures without a specific provoking cause, and more than 20 different antiepileptic drugs are currently used in its treatment. However, because drug response varies from patient to patient, many individuals must go through repeated switches of ineffective medications.
In fact, it is known that about 30% of all patients show a refractory course, failing to respond even after two or more adjustments of their medication regimen.
The researchers analyzed baseline clinical information and follow-up data of more than three years from approximately 2,600 patients with epilepsy who were treated at Seoul National University Hospital between 2008, when a new epilepsy classification system was introduced, and 2017. The analysis included a total of 84 variables, such as antiepileptic drug history, seizure type, brain Magnetic Resonance Imaging (MRI) and electroencephalography findings, blood test results, and treatment course.
The machine-learning model applied a tree-based ensemble method, and treatment response was defined as a reduction of at least 50% in seizure frequency after initiation of an antiepileptic drug.
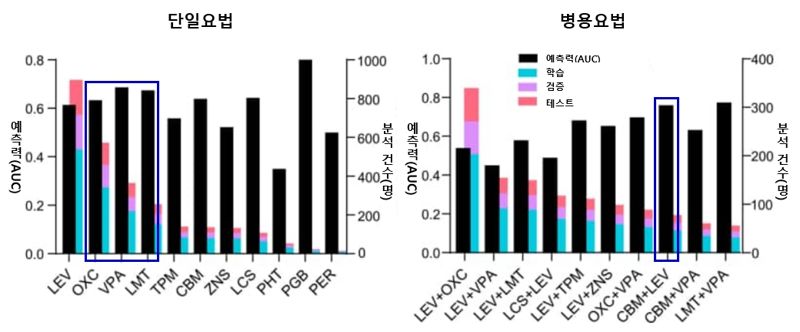
The main drugs analyzed were levetiracetam (LEV), Oxcarbazepine (OXC), Valproic acid (VPA), and lamotrigine (LMT), all of which are commonly prescribed in clinical practice.
In monotherapy, Valproic acid (AUC 0.686) showed the highest predictive performance for treatment response, followed by lamotrigine (0.674) and Oxcarbazepine (0.633). Among combination therapies, the regimen combining Carbamazepine and Levetiracetam (CBM+LEV) demonstrated the highest predictive power, with an AUC of 0.764.
The team also used Shapley Additive Explanations (SHAP) to identify key clinical factors influencing treatment response to each drug. They found that patients with generalized tonic-clonic seizures were more likely to respond to Valproic acid, while those with late-onset epilepsy or a shorter disease duration had a higher probability of responding to lamotrigine. These findings suggest that the clinical determinants of treatment response differ from one antiepileptic drug to another.
“Until now, the choice of antiepileptic drugs has largely depended on the specialist’s experience and a process of trial and error,” PARK Kyung-Il of the Department of Neurology at Seoul National University Hospital noted. “This study is meaningful in that it demonstrates the possibility of predicting treatment response to specific drugs in advance, based on large-scale clinical data,” he explained. He added, “We plan to further expand the dataset with multi-center data and develop this into a tool that can support treatment decisions in real-world clinical settings.”
The study findings were published in a recent issue of Scientific Reports, an international journal in the Nature family.
vrdw88@fnnews.com Kang Jung-mo Reporter